AI-Driven Healthcare Revenue Cycle Management Services
Our advanced RCM technology and healthcare revenue cycle management software help practices collect faster, cut denials, and stay compliant.

Trusted by today’s leading healthcare organizations
|
|
 |
 |
 |

Overcome Revenue, Staffing, and Compliance
Challenges with RCM Solutions
You want to lead your practice toward stronger financial performance and streamlined operations—but it’s nearly impossible to have in-house experts for every step of the revenue cycle. That’s why you need a trusted revenue cycle management company that delivers end-to-end support.
Since 1977, ADS has been providing healthcare organizations with reliable revenue cycle management services and solutions, helping clients reduce costs, increase collections, and achieve sustainable growth.
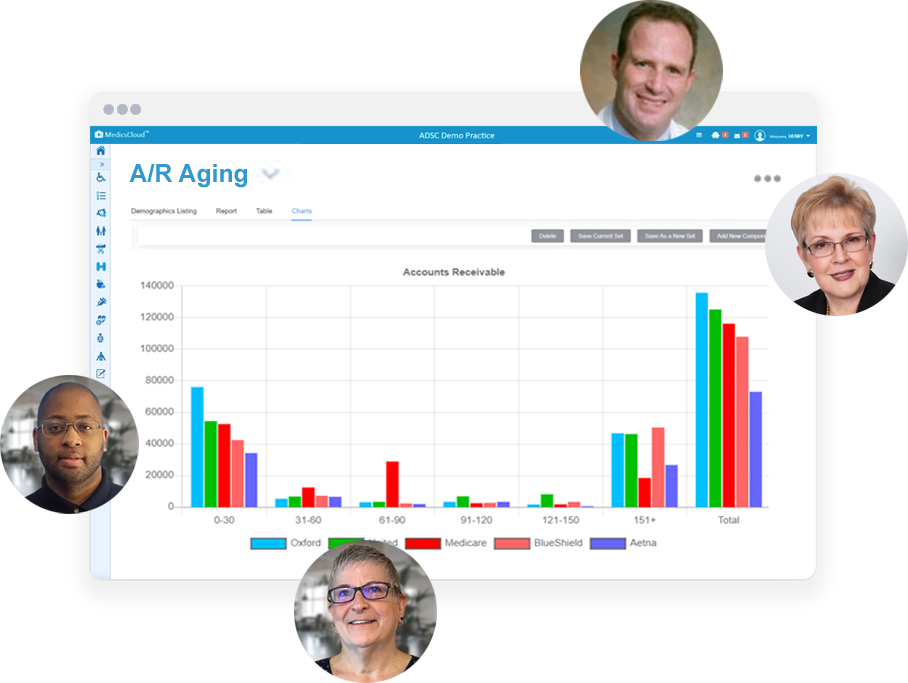
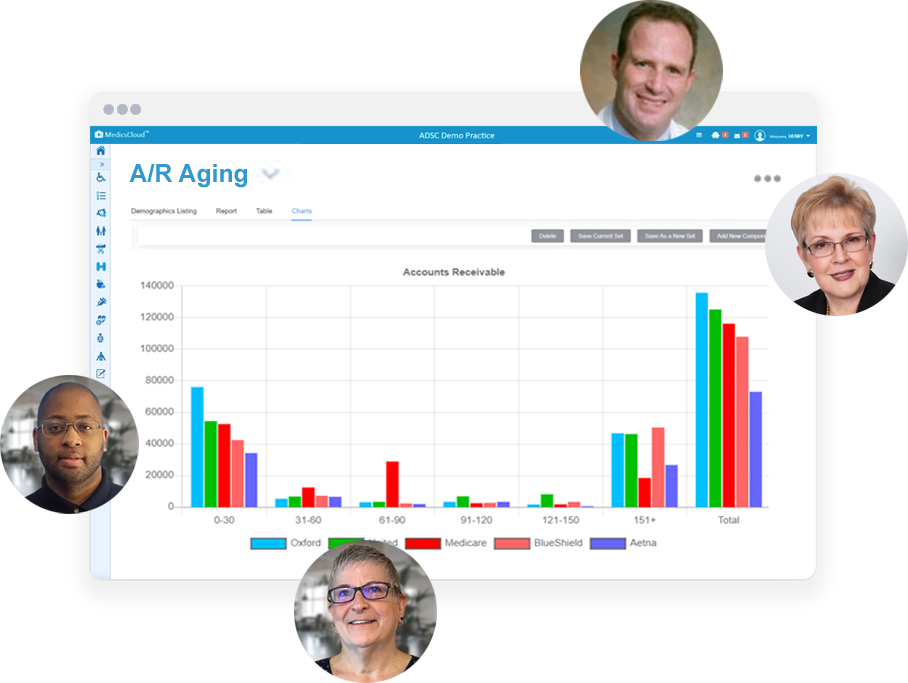
"Our revenue increased by 24% in the first year, and denials were reduced by 20% after 120 days."

David Fischler, M.D.
Pulmonary and Intensive Care Specialists
"Our revenue increased by 20% in the first 6 months with 97% of A/R being under 60 days."

Russell Samofal, M.D.
Podiatry Center of New Jersey
"Our A/R dramatically reduced 30% after the first 90 days. Denials have been reduced by 10% to 15%."

Gladys Serrano, CEO
Hispanic Counseling Center (HCC)
Evaluate Your
Revenue Cycle Management Performance
Tracking these key revenue cycle management metrics—and applying process improvement strategies—helps healthcare organizations boost collections, reduce denials, and strengthen overall financial performance.
98%
Authorization Capture
99%
Clean Claim Rate
(First Pass)
98%
Verified Insurance Eligibility Success
< 48
Hour Claim Submission
< 5%
Denial Rate
< 30
Target A/R Days
90%
Collections within
90 Days
96%
Collections within 120 Days
< 30%
Self Pay A/R
< 3%
Bad Debt
Step-by-Step: How Our
RCM Services Improve Your Revenue Cycle
Every step of the patient journey is supported by our revenue cycle management technology, ensuring cleaner claims, faster payments, and maximum revenue capture.
Credentialing
Registration
Prior Authorization and Eligibility
Charge Entry and Coding Review
Claim Scrubbing and Submission
Automated Denial and Appeals Management
Payment Posting and Patient Collections
Weekly Performance Review
Increase Revenue, Lower Costs, and Transform Your Revenue Cycle Management Experience
A team of 300+ billing and workflow professionals works behind the scenes for you to alleviate your staffing issues while maintaining:
- 40+ years of revenue cycle and billing services experience
- an average collection rate of ~96% across all our RCM clients
- Claims are submitted at their highest possible value
- Out-of-network alerts on scheduling
- Automated eligibility verification and insurance discovery
- denial resubmissions within 48 hours
- proactive denial alerts help to avoid them in the first place
- immediate statements to patients and online payment options
- patients contact us – not you – with statement questions
MedicsRCM can connect with virtually any EHR, hospital, PM, G/L, PACS, or LIS.
Improve Cash Flow and Shorten A/R Cycles Using AI-Driven RCM Solutions
You’ll benefit from our proven RCM services model to deliver real results:
- Achieve an average collection rate of ~96%
- Improve your clean claim submission rate, reduce denials, and provide more accurate/timely payment posting
- Collect more of what's NOT being paid including denials, appeals, and open patient balances
Simplify Compliance with CMS Rules and Industry Requirements
You won’t have to worry about the seemingly never-ending billing regulations affecting your practice including:
- No-Surprises Act
- Cures Act
- Clinical decision support
- MIPS reporting
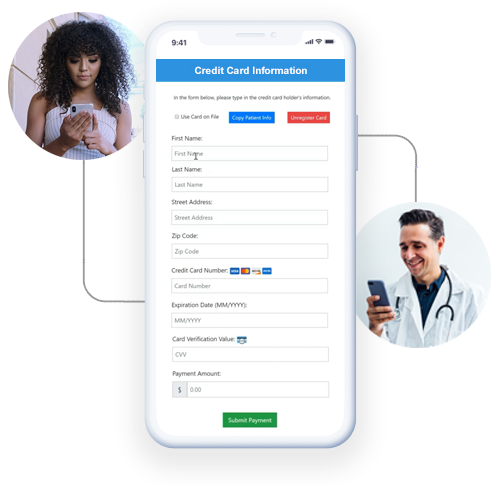
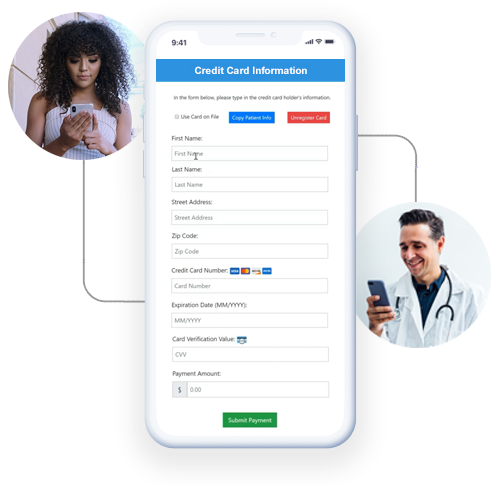
Simplify Patient Payments with Revenue Cycle Management Solutions
Use an array of features that work to reduce your outstanding patient balance A/R including:
- access to a patient responsibility estimator
- enabling patients to pay from any mobile device
- interactive balance due reminder texting

Protect Patient Data with Secure RCM Technology
When patient information is involved, HIPAA can respond with severe financial penalties if you don’t have protections in place. So, we take our clients’ security very seriously.
- 99.9% Uptime
- HIPAA Compliant
- SOC-1 & SOC-2
- Disaster Recovery


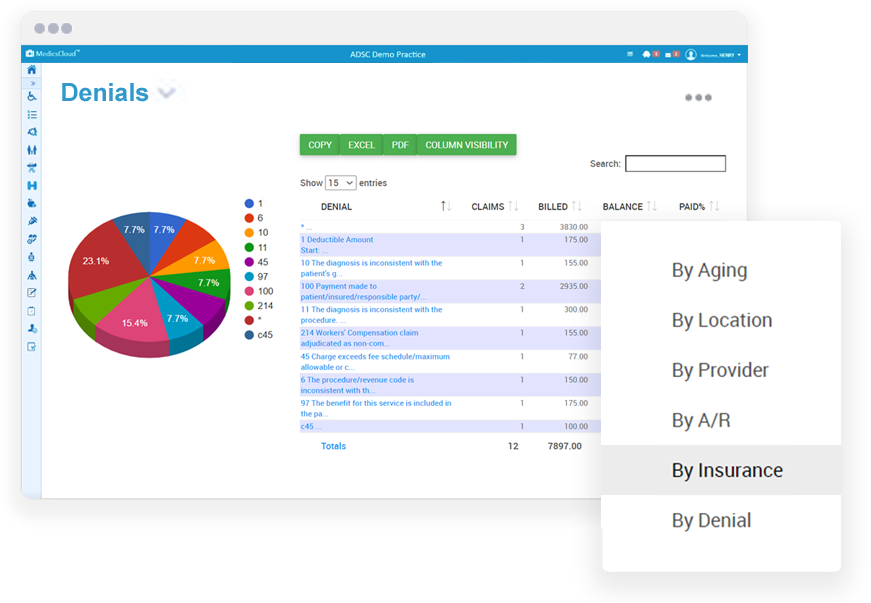
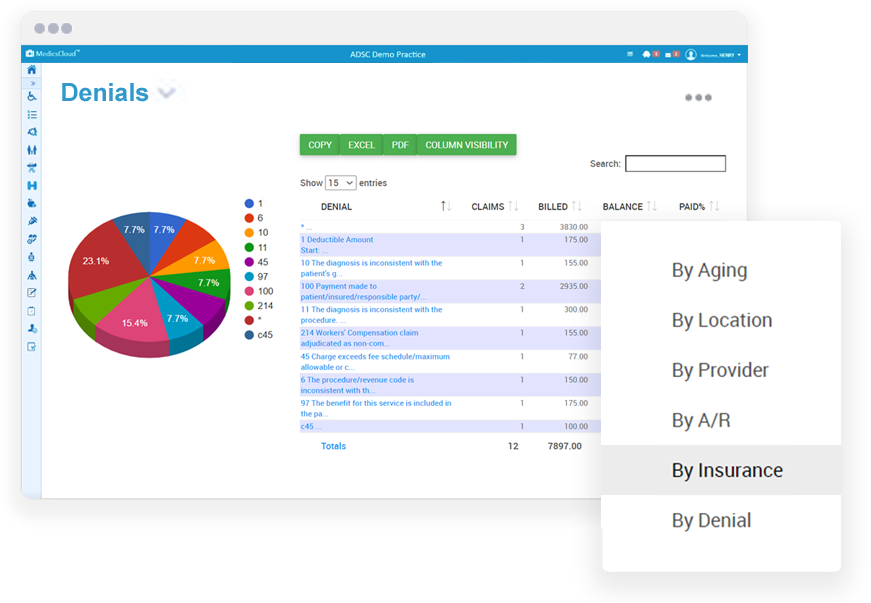
Track and Improve Your Revenue Cycle Management Results
Following MGMA financial reporting recommendations, you'll be provided key industry metrics and process improvement strategies to improve your revenue cycle. We'll meet with your team weekly and monthly to review your key:
- Benchmarking metrics
- Key Performance Indicator (KPI) metrics
- Best practices for billing

What Healthcare Providers Say About Our RCM Services
"Working with MedicsRCM has proven to be a very professional experience for my staff, giving them the ability to turn to a single source, and to get any questions quickly answered. Most importantly, reimbursements have gone up! Overall, MedicsRCM has made the practice so much better."
Thomas Beggins, MD | Connecticut Eye Physicians PC
Put our experience to work for you
Our management team has over 200 combined years of experience in RCM and billing services.

Sheryl Miller, MBA
EVP of Sales & BD, RCM Services

Gene Spirito, MBA
National Sales Manager, RCM
.png?width=231&height=170&name=Jim-ONeill-Lab%20(1).png)
Jim O'Neill
Sales Manager, Laboratory RCM
.png?width=231&height=170&name=Scott-Friedman-BH%20(1).png)
Scott Friedman
Director of Sales, RCM Division

Marybeth McGowen
RCM Division Manager

Daphna Barzillai, MBA
RCM A/R Manager

Isaiah Leech, MBA
National Portfolio Manager

Kim Becker
National Portfolio Manager
Getting started with RCM services
Achieving dramatic business growth is as easy as 1, 2, 3...

1. Talk with an Advisor
Tell us your financial and operational goals, get your questions answered, and discover how much our team can increase your revenue and efficiency.

2. Develop a Plan
Our proven process has increased our clients’ revenue typically by 10% -20% and sometimes even more. Together, we'll build a perfect plan for you.

3. Experience Success
You’ll see increased revenue, have more money in the bank, and operate more efficiently. In fact, our 90-day guarantee guarantees it!
How much do our RCM services cost?
MedicsRCM cost generally ranges from 3% to 6% based on the collection amount. However, your fee can actually be 0% when factoring in how:
- your technology spend is reduced or eliminated with our financial/management platform and cloud hosting included as part of our service
- your in-house staffing and operational costs are consolidated with our team of 300+ billing and EDI experts
- your revenue is guaranteed to increase in 90 days over whatever healthcare revenue cycle management company or in-house system you’re currently using
The sum total on the points above = more income to you even with our fee factored in!
Revenue Cycle Management - FAQs
Selecting a revenue cycle management services company can be difficult. You probably have loads of questions, so let’s get you started on some of the most frequently asked questions we get.
How long does it take to transition to your healthcare RCM service?
We can start to submit your claims in as little as 30 days once our 5-7 days of testing is completed.
Will I have single or multiple points of contact with your RCM service?
A MedicsRCM Services Manager, experienced in your specialty(ies), is assigned under which following resources operate:
- Dedicated Account Manager
- Billing Team Members
- EDI specialists for claims, remittances, EOB reconciliations, eligibility verifications, and direct fund deposits
- HL-7 interface specialist
- A senior member of the ADS management team is also connected with each MedicsRCM client
How will my current databases be handled?
We import your current files such as Referring Physician, Insurance, and Fees into our MedicsPremier practice management system.
Does your healthcare RCM service start sending our claims from Day One?
No one wants to submit all of your claims more than we do since we only get paid on amounts collected. But, that would be irresponsible. Instead, we submit test claims for 50 to 100 of your patients for approximately 5 to 7 days. All of your claims are submitted once the test claims are verified.
What happens if my current RCM company stops submitting our claims?
We can bill and resubmit claims from your current medical revenue services team to expedite patient payments. In fact, MedicsRCM tracks old claims vs. new claims.
Do we have access to our data?
Yes, MedicsRCM clients have 24 x 7 on-demand cloud access to all of their data so they can truly understand healthcare costs. We train clients on using our MedicsPremier system, and encourage them to see how things are going! Healthcare revenue cycle management should not be behind locked doors.
What if we need customized management reports?
Healthcare providers almost never need truly customized reports since our reports/dashboards as so highly user-defined and are exportable to Excel. But if a certain customized report(s) are needed, your Accounts Team will provide same via standard PDF or Excel.
Are forms needed for electronic claims?
Possibly, and if so, we provide you with whatever form(s) are needed by any insurance payer(s) and provide assistance, if needed, in completing them. Of course 100% electronic claims and EOB reconciliations - which our team handles for you - are encouraged.
Does your RCM service have tools for mobility and engagement?
Yes, with our options for Medics Telemedicine, Portal, Texting, Kiosk for expedited intake, and even for remote patient monitoring (RPM) of vitals. Telemedicine and RPM are ideal for generating revenue and texting keeps patients tuned into their in-office and telemedicine appointments while helping to eliminate no-shows. And we're always looking forward at revenue cycle management trends.
Can we use an EHR with your revenue cycle management service?
Yes, we actually have three options for EHR! (1) Use your existing EHR interfaced with our MedicsPremier platform. (2) Use the MedicsCloud EHR, excellent for almost any specialty and which is almost always at no additional cost. (3) Use our electronic superbill if you prefer to not use an EHR at all, or if you’d rather not have yours interfaced with us for whatever reason.
Keep up with the latest RCM and billing trends, insights, and industry news
Medical Billing / RCM | Laboratory
Patient Financial Engagement Starts at Intake: Why Front-End Patient Access Is Now a Revenue Strategy
For years, patient financial engagement was treated as a collections problem. In 2026, that framing ...
By Jim O'Neill
on January 16th, 2026
Medical Billing / RCM | Laboratory
2026 Laboratory Billing Trends: Why In-House Teams Are Struggling — and How AI Is Changing RCM
In 2026, laboratory billing teams are facing a perfect storm.
By Jim O'Neill
on January 15th, 2026
Medical Billing / RCM | Laboratory
What Challenges Are Laboratories Facing in Revenue Cycle Management in 2026?
Laboratory revenue cycle management has never been simple — but in 2026, it has become structurally ...
By Christina Rosario
on January 14th, 2026